Is the number of chromosomes in the embryo we want to place in the woman correct?
Genetic testing is a technology that examines the DNA of embryos in the embryology laboratory and is an alternative to Prenatal Genetic Diagnosis since the late 1980s. It was created to help couples at risk of passing on a hereditary disease to their offspring.
The reason for creating this technology is that embryos with the correct number of chromosomes (euploid) have a better success rate than those with the incorrect number of chromosomes (aneuploid).
Chromosomes are the carriers of DNA. We have 46 chromosomes – 23 come from the egg and 23 from the sperm. Twenty-two of them are "autosomal" and 2 are sex chromosomes (X and Y). All 46 chromosomes carry the DNA molecule, which gives all the necessary instructions to cells for life and normal functioning.
Sex chromosomes determine our biological sex. A woman carries two X chromosomes and a man has one X and one Y chromosome.
Cells that have a different number of 46 chromosomes are aneuploid. For example, an embryo in which all cells are 45 is aneuploid. An embryo with 46 chromosomes is euploid, i.e. has the correct number of chromosomes.
If your embryo is aneuploid, it has a high chance of failing to implant, or after implantation, of being aborted at a later stage.
Aneuploidy most often results from errors during the maturation of eggs and sperm. So, for example, instead of getting 23 chromosomes in a sperm, an error can occur resulting in 22 chromosomes. Thus, when combined with an egg with 23 chromosomes, an embryo with 22+23=45 chromosomes, making it aneuploid.
These errors may occur more frequently with age and are related to egg and sperm quality.
Eggs are much more likely to be aneuploid with age, and embryos from them will also be aneuploid.
For women who have undergone repeated miscarriages (two or more), those with several unsuccessful in vitro attempts, or those over the age of 35, and if they are with partners with severely impaired sperm quality, genetic testing of the embryos before implantation could be useful.
How is the testing done?
A few cells (5-10) must be taken from the embryo - a biopsy.
In modern practice, embryos are cultured for 5-6 days in the laboratory until reaching a stage of development called a blastocyst.
The procedure consists of several steps:The procedure consists of several steps:
- A small opening is made with a laser in the shell of the three-day-old embryo - this is Assisted Hatching.
- By day 5, 6, or 7, a few cells from the blastocyst begin to poke through the opening.
- These cells are separated from the embryo with the help of a laser – a biopsy material is obtained.
- The biopsy material is sent to a genetics laboratory for testing.
- The embryo is frozen until the results are available, and then a transfer date is scheduled.
What might the results of the biopsy be?
Genetic testing shows the number of chromosomes in the embryo.
The possible outcomes are broadly divided into three categories:
- Euploid embryo – correct number of chromosomes. This embryo is a priority for transfer.
- Aneuploid embryo - incorrect number of chromosomes. Such an embryo is avoided.
- Mosaic embryo - where part of the cells have the correct number of chromosomes, and another part has an incorrect number. Depending on the severity of the damage, it is assessed whether and in what order (if there are other embryos) it can be returned to the woman.
Genetic testing is a selection technology independent of the traditional culture approach up to day five (blastocyst stage), but combined with it, it provides important additional information about the quality of the embryos and helps us make a better-informed transfer decision.
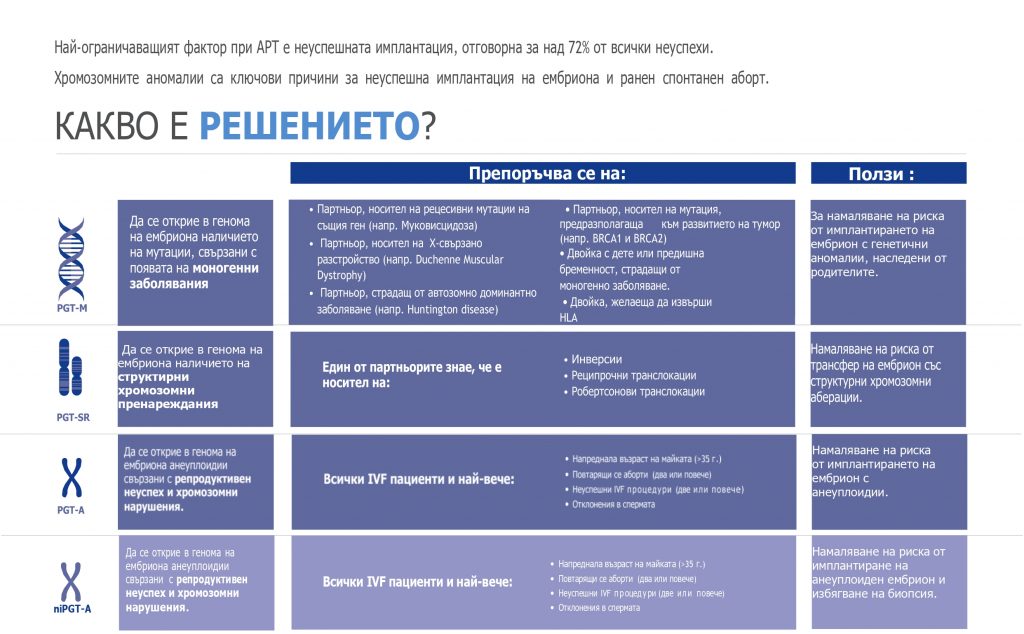
Preimplantation genetic diagnosis of embryos:
PGT-A – Aneuploidies
PGT-SR – Structural chromosomal rearrangements
PGT-M – Monogenic diseases
niPGT-A – Non-invasive genetic diagnosis for aneuploidies